- Introduction to Subjective Methods
- Birth weight
- Body shape
- Weight and height
- Waist and hip circumference
- Introduction to Objective Methods
- Simple measures - stature
- Simple measures - weight
- Simple measures - circumference
- Simple measures - arm anthropometry
- Simple measures - skinfolds
- Simple measures - abdominal sagittal diameter
- Simple measures - head circumference
- Bioelectric impedance analysis
- Multi-component models
- Hydrostatic underwater weighing
- Air displacement plethysmography
- Hydrometry
- Whole body DEXA scan
- Near infrared interactance
- Whole body counting of total body potassium
- 3d photonic scan
- Magnetic resonance imaging (MRI) / Magnetic resonance spectroscopy (MRS)
- Total body electrical conductivity (TOBEC)
- Computed tomography (CT)
- Ultrasonography
- Introduction anthropometric indices
- Body mass index
- Fat and fat free mass indices
- Ponderal index
- Percentiles and Z-scores
- Anthropometry Video Resources
- Height procedure
- Protocol for measuring waist circumference
- Measuring hip circumference
- Weight and body composition procedure
Percentiles and Z-scores
Percentiles and Z-scores are a widely used format to display and interpret growth measurements. In childhood, sex and age-adjusted percentiles and Z-scores for weight, height (supine length if aged less than two years), BMI and ponderal index (at birth) are routinely used in clinical practice and in research studies. These values are used to assess growth and nutritional status in infancy, childhood and adolescence (up to 19 years of age) They are derived by comparing individual growth measurements against growth data or growth charts from a reference (‘normal’) population (a “growth reference” or “growth standard”).
- Percentile indicates the percentage of observations that fall below a certain value.
- Z-score is the distance and direction of an observation away from the population mean.
To calculate percentiles and Z-scores, you need:
- The measurement value of the child’s weight, height (supine length if aged under two years), BMI or ponderal index (at birth). The unit of the measurement should be clearly stated to avoid errors (most growth reference data are provided in metric units).
- The child’s sex and their age at time of the measurement.
- Growth data or growth charts from a reference population (a “growth reference” or “growth standard”) that is appropriate for the child’s background.
Percentiles and Z-scores are routinely used in clinical practice to assess and monitor children’s growth and nutritional status and are also widely used in the analysis of data from child nutrition surveys and epidemiological studies. The following indices are expressed as percentiles or Z-scores:
- “Weight-for-age” indicates a child’s body weight for their age and sex relative to the reference population. It is an important indicator of a child’s nutritional status, such as underweight or overweight in young children aged less than two years old.
- “Height (or length)-for-age” indicates a child’s height (or supine length in children less than two years old) for their age and sex relative to the reference population. It is used in clinical practice to monitor a child’s growth and is influenced by genetic potential (parents’ heights), nutritional factors, and the ‘tempo’ of growth, which is a measure of how rapid or slow in timing to achieve final adult height and is closely related to puberty timing.
- “BMI-for-age” indicates a child’s BMI for their age and sex relative to the reference population. It is used (usually in children aged older than two years) to indicate weight status independent for height, and is used to define childhood overweight, obesity and thinness categories.
- “Weight-for-height (or length)-for-age” indicates a child’s weight status independent of their height relative to a reference population, typically in children aged under two years old. It is often used to indicate whether children are overweight, obese or underweight. (Note: these indices are often referred to as simply “weight-for-height” and “weight-for-length”).
- At birth, percentiles and Z-scores for a newborn infant’s weight, length and ponderal index are usually adjusted for sex and gestational age at birth. These are used to indicate the rate of fetal growth during pregnancy.
- Z-scores are also often used to ‘clean’ large datasets by excluding outlying data. Z-scores that lie outside +/- 4, 5 or 6 might be considered to be implausible and are changed to missing values.
Percentiles
In clinical practice, growth percentiles are commonly derived by manual plotting of the child’s growth measurement against their age on a sex-appropriate paper growth chart to visually indicate their approximate percentile position or band (e.g. “between 85th to 97th”) (see Figure 1).
Alternatively, percentiles can be more precisely converted from Z-scores (see section below).
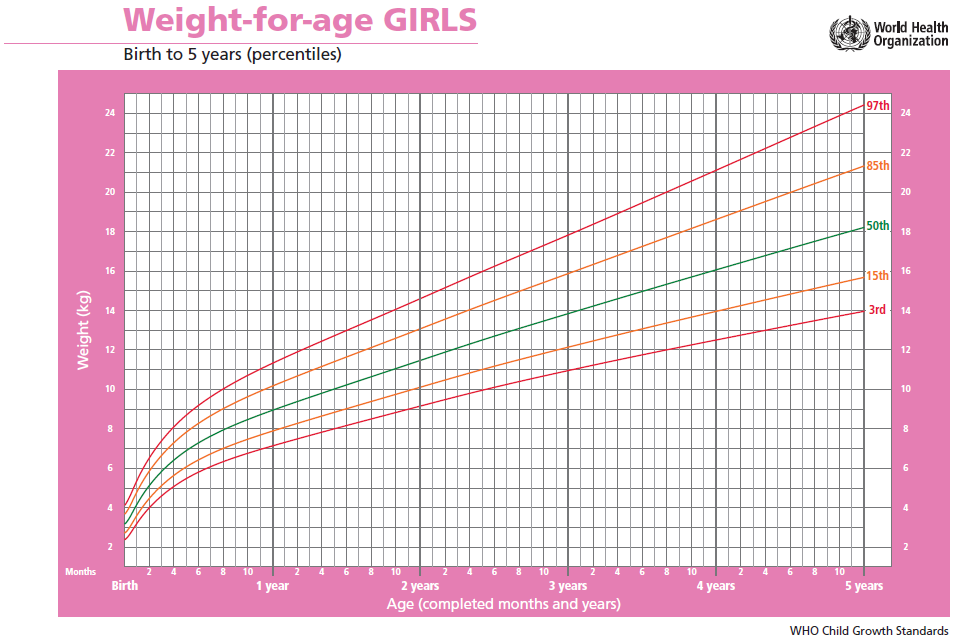
Figure 1 WHO Child Growth Standards Weight-for-age: Birth to 5 years percentiles chart for girls.
Source: http://www.who.int/childgrowth/standards/chts_wfa_girls_p/en/
Z-scores
A Z-score is calculated using the formula (assuming a normal distribution):
Measured value – Average value in the reference population
Standard Deviation of the reference population
Average values and standard deviations for various reference populations are available adjusted for age and sex and indicating the appropriate transformation to achieve a normal distribution (see below).
Calculation of Z-scores by hand is laborious. Fortunately, several computer programs are available and data can be entered either one child at a time or using spreadsheets for large numbers of children (e.g. http://www.who.int/childgrowth/software/en/).
It is very important to note the units of measurement required by each of the programs. For example: weight in kg; height/length in cm; age in decimal years, months or days; and sex as M for male and F for female.
Percentiles and Z-scores are easily interchangeable using a table of Z-scores and their associated areas (percentile = the area from infinity to Z) or a calculator.
In Microsoft Excel: To convert Z-scores to percentiles, use the Norm.Dist function with the settings: mean=0; SD=1; cumulative=TRUE.
Which growth reference?
It is important to select the reference population carefully, with consideration of the aim of the assessment or study. For example, older growth reference data might be appropriate if analysing data from an historical study or survey, or to assess secular trends in growth.
Some countries (e.g. UK, USA, and several other European countries) have growth reference data based on their national population (see below). Such growth references are representative of children in those populations. Hence, these percentiles and Z-scores tell you where a measured child lies in relation to that population, but they do not imply that a normal growth value or pattern is healthy.
WHO International Growth Standards and Growth References
The World Health Organisation (WHO) provides international growth standards for children aged 0-5 years and international growth references for children and adolescents aged 5-19 years. While both are intended to be used for children of any nationality, there is an important distinction between standards and references.
- The WHO Child Growth Standards 0-5 years are based on data from the WHO’s large prospective Multinational Growth Reference Study (MGRS), which followed children growing in optimal environmental and health conditions in six countries. Growth standards describe an optimally healthy growth pattern that steers a middle-ground between undernutrition and overnutrition. They do not necessarily provide a good statistical fit to each country, e.g. in an ‘overnourished’ population the large majority of children may lie above the 50th percentile for weight and BMI.
- The WHO Growth Reference for 5-19 years is a reconstruction of 1977 national US growth data. It is intended for use in populations who do not have appropriate national growth data.
Preterm infants
Birth weight and birth length reference data are available for preterm infants born from 24 weeks gestation onwards. For example, the INTERGROWTH-21st growth references.
For assessments of postnatal growth, prematurity needs to be taken into account. Age-adjustment is for children born before 37 weeks gestation. For example, if an infant is born 6 weeks early (at 34 weeks gestation), he/she will have a corrected age of 6 weeks less than his/her actual age since birth (compared to 40 weeks of gestation).
Many growth computer softwares will adjust for gestational age. When manually plotting measurements onto a chart, their measurements should be plotted at their actual age, with a horizontal line drawn back to their corrected age. The adjustment should continue to be made until the child is one year old.
The Preterm Postnatal Growth Standards are particularly suitable for monitoring postnatal growth in preterm babies after 32 weeks’ postmenstrual age and may be used for the assessment of preterm infants until 64 weeks’ postmenstrual age (6 months “corrected” age), the time at which they overlap, without the need for any curve adjustment, with the WHO Child Growth Standards for term newborns.
Growth categories based on percentiles and Z-scores
To identify individuals with unhealthy growth: the WHO recommends cut-off values of +/- 2 Z-scores, which roughly correspond to the 2nd and 98th percentiles (Table 1).
Table 1 WHO classification of growth and nutritional status.
|
|
cut-off points |
cut-off points |
|
|---|---|---|---|
| Based on weight and height indices | Height-for-age < -2SD to -3SD | Height-for-age < -2SD to -3SD | Stunted |
| Height-for-age < -3SD | Height-for-age < -3SD | Severely stunted | |
| Weight-for-age < -2SD to -3SD | Weight-for-age (up to 10 years) < -2SD to -3SD | Underweight | |
| Weight-for-age < -3SD | Weight-for-age (up to 10 years) < -3SD | Severely underweight | |
| Weight-for-height < -2SD to -3SD | Wasted | ||
| Weight-for-height < -3SD | Severely wasted | ||
| Based on body mass Index (BMI) | BMI-for-age (or weight-for-height) > 1SD | Possible risk of overweight | |
| BMI-for-age (or weight-for-height) > 2SD | BMI-for-age > 1 SD (equivalent to BMI 25 kg/m2 at 19 years) | Overweight | |
| BMI-for-age (or weight-for-height) > 3SD |
BMI-for-age > 2SD (equivalent to BMI 30 kg/m2 at 19 y) |
Obese | |
| BMI-for-age < -2 to -3 SD | Thin | ||
| BMI-for-age < -3 SD | Severely thin |
1 Z-score and percentile equivalence: 3SD=0.1%; 2SD=2.3%; 1SD=15.9%; +1SD=84.1%; +2SD=97.7%; +3SD=99.9%.
Adapted from: http://ebook.ecog-obesity.eu/chapter-growth-charts-body-composition/world-health-organization-reference-curves/
To assess and monitor the prevalence of overweight and obesity in populations:
As shown in Figure 2, the (UK) National Child measurement programme (NCMP) and some other national organisations use the BMI-for-age 85th and 95th percentiles cut-offs (equivalent to Z-scores of +1.04 and 1.65, respectively).
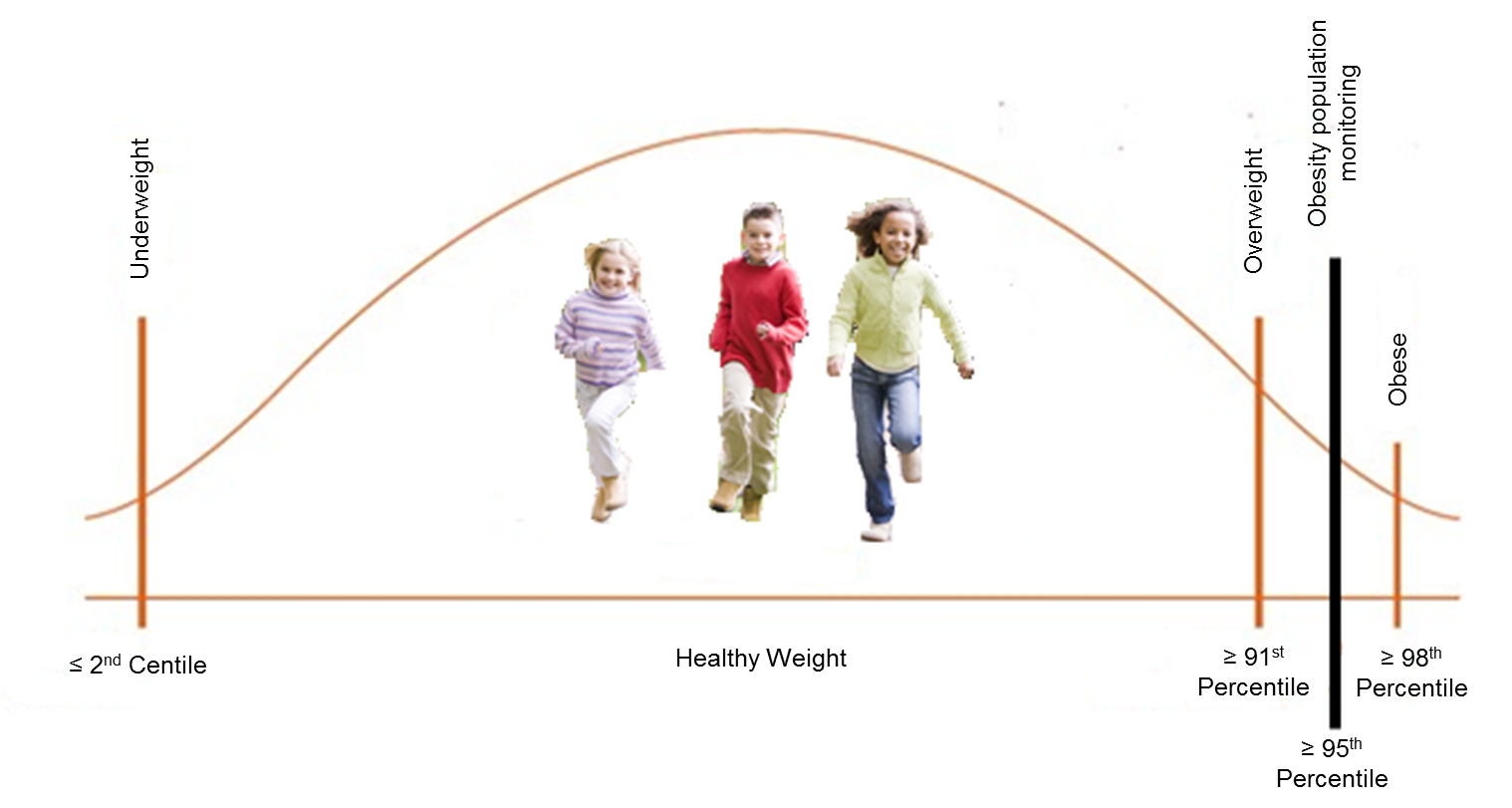
Figure 2 Individual and population cut-off values for BMI-for-age percentiles used in the UK.
Strengths
- Easy to calculate.
- Inexpensive.
- Non invasive.
- Standardised cut-off points available.
- Strongly correlated with body fat levels measured by direct/objective methods.
- BMI can be used to track body size throughout the life cycle. This is important because BMI-for-age in childhood is a determinant of adulthood BMI.
- BMI-for-age relates to health risks and correlates to direct measures of adiposity measured by DEXA.
- BMI-for-age captures changes in the weight-height relation with age and can be used continuously up to the age of 18.
- Weight-for-height easier to understand and to calculate than is BMI.
- Weight-for age is the most commonly used indicator, but is more effective when the trend over age for the same child is studied. This trend is compared with the trend seen in healthy subjects in that population. The assessment is population specific.
Limitations
- WHO weight-for-age reference data are not available beyond age 10, because this indicator does not distinguish between height and body mass in an age period where many children are experiencing the pubertal growth spurt and may appear as having excess weight (by weight-for-age) when instead they are tall.
- The weight-to-height relationship changes dramatically with age and with maturation status. As a result, at a given height, the weight corresponding to a particular percentile is not the same for all ages, so that the meaning of a given weight-for height percentile differs according to age.
- Weight-for-age fails to distinguish a thin but tall child from a well-proportioned child.
- Prevalence of problematic growth or nutrition status patterns can be different when estimated based on different growth references/standards.
- Racial or ethnic differences and secular trends in growth, body composition, body build, and sexual maturation are likely to complicate the interpretation of anthropometric measures and cut-off points.
- The use of inappropriate growth charts will affect the interpretation of those indices possibly resulting in mis-classification of the population nutritional status and inaccurate evaluation of child growth trajectories.
- These indices are not direct measurements of body composition. Among relatively heavy children, BMI is a good indicator of excess body fatness; however, among relatively thin children (those with a BMI-for-age of <85th percentile), BMI is more an indicator of fat-free mass.
- Other variables are required e.g. age, sex, gestational age may be required for their interpretation. In children height, sexual maturation and age influence the relationship between BMI and body fat. For this reason, for infants, children and adolescents, BMI and weight for height indices have to be interpreted relative to a child's age and sex.
- For children and teens, BMI is not a diagnostic tool and is used to screen for potential weight and health-related issues. For example, a child may have a high BMI for their age and sex, but to determine if excess fat is a problem, a health care provider would need to perform further assessments. These assessments might include skinfold thickness measurements, evaluations of diet, physical activity, family history, and other appropriate health screenings. The American Academy of Pediatrics recommends the use of BMI to screen for overweight and obesity in children beginning at 2 years old.
- The accuracy of this index in children and adolescents varies according to individual’s degree of fatness:
- Poor indicator in overweight children as a high BMI may be due to increased level of fat or fat free mass
- Poor Indicator in thin children as differences in BMI are often due to differences in fat free mass
Considerations relating to the use of percentiles and Z-scores in specific populations are described in Table 2.
Table 2 Application of percentiles and Z-scores in different populations.
| Population | Comment |
|---|---|
| Pregnancy | Not used. |
| Infancy and lactation | Suitable. |
| Toddlers and young children | Suitable. |
| Adolescents | Suitable. |
| Adults | Not used – BMI typically implemented |
| Older Adults | Not used – BMI typically implemented |
| Ethnic groups | Suitable in infancy, childhood and in adolescents. Use a population-appropriate growth reference. |
| Other (obesity) | Suitable in infancy, childhood and in adolescents. For extreme values, Z-scores are more informative than percentiles. |
Refer to section: practical considerations for objective anthropometry
Resources are dependent on the instruments/methods used to derive the raw data (weight and height), however computer and freely available software are recommended to derive the scores.
WHO
WHO growth reference for school-aged and adolescents.
USA
CDC growth charts from birth to 20 years in the United States web page and PDF.
UK
UK 1990 growth reference: British growth reference, anthropometric data for weight, height, body mass index and head circumference from 17 distinct surveys representative of children in England, Scotland and Wales in 1990.
May 2009 The UK-WHO (2006) growth reference for 0-4 years old children also suitable for moderately preterm infants (32-36 weeks gestation).
May 2009 The UK-WHO growth reference for 2-18 years old children and adolescents.
They intend to assess the growth of school age children and young people in primary or secondary care. The chart includes guidance on the onset and progression of puberty, a BMI centile lookup.
The programmes/macros (LMS macros) for these references can be downloaded here.
Italy
The Italian Society for Pediatric Endocrinology and Diabetes (SIEDP)-2002 growth charts for height, weight and body mass index (BMI), to obtain charts (SIEDP-2006) that apply to the Italian population from 2 to 20 years of age, taken as a whole, or separately in two geographical areas (Central-North Italy and South Italy). See here for software and PDF.
Denmark
Updated in 2014, these include references for height/length, weight and head circumference from 0 to 20 years of age.
Sweden
Updated in 2002, these include references for height/length, weight and head circumference from 0 to 10 years of age.
Syndrome-specific growth references
Reference charts for syndromes with endocrine features are available for Down Syndrome, Turner syndrome and Achondroplasia. This software also contains over 200 growth charts for different geographical regions. However, charges are applied for its use.
- Cole TJ. The LMS method for constructing normalized growth standards. European journal of clinical nutrition. 1990;44(1):45-60. Epub 1990/01/01.
- Flegal KM, Wei R, Ogden C. Weight-for-stature compared with body mass index-for-age growth charts for the United States from the Centers for Disease Control and Prevention. The American journal of clinical nutrition. 2002;75(4):761-6. Epub 2002/03/28.
- Ong KK. WHO Growth Standards - Suitable for Everyone? Yes. Paediatric and perinatal epidemiology. 2017;31(5):463-4. Epub 2017/08/26.
- Wang Y, Chen H. Use of Percentiles and Z-Scores in Anthropometry. Neonatal anthropometry: a tool to evaluate the nutritional status, and to predict early and late risks: Springer, Editors: Victor R. Preedy; 2012. p. 29-48.
- Wang Y, Moreno LA, Caballero B, Cole TJ. Limitations of the current world health organization growth references for children and adolescents. Food and nutrition bulletin. 2006;27(4 Suppl Growth Standard):S175-88. Epub 2007/03/17.
- Wright C, Lakshman R, Emmett P, Ong KK. Implications of adopting the WHO 2006 Child Growth Standard in the UK: two prospective cohort studies. Archives of disease in childhood. 2008;93(7):566-9. Epub 2007/10/03.
- https://www.cdc.gov/nccdphp/dnpao/growthcharts/who/methodology/index.htm
- http://conflict.lshtm.ac.uk/page_121.htm#Malnutrition_Anthropometry_Indices
- http://www.who.int/childgrowth/standards/technical_report/en/
- https://www.who.int/tools/child-growth-standards
- http://ebook.ecog-obesity.eu/chapter-growth-charts-body-composition/world-health-organization-reference-curves/
- http://www.gosh.nhs.uk
- https://www.who.int/toolkits/child-growth-standards/standards
- http://www.medicalbiostatistics.com/childhealth.pdf
- https://www.unicef.org/progressforchildren/2006n4/index_survivalanddevelopment.html
- https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html
- http://www.who.int/childgrowth/software/en/
