- Introduction to Subjective Methods
- Birth weight
- Body shape
- Weight and height
- Waist and hip circumference
- Introduction to Objective Methods
- Simple measures - stature
- Simple measures - weight
- Simple measures - circumference
- Simple measures - arm anthropometry
- Simple measures - skinfolds
- Simple measures - abdominal sagittal diameter
- Simple measures - head circumference
- Bioelectric impedance analysis
- Multi-component models
- Hydrostatic underwater weighing
- Air displacement plethysmography
- Hydrometry
- Whole body DEXA scan
- Near infrared interactance
- Whole body counting of total body potassium
- 3d photonic scan
- Magnetic resonance imaging (MRI) / Magnetic resonance spectroscopy (MRS)
- Total body electrical conductivity (TOBEC)
- Computed tomography (CT)
- Ultrasonography
- Introduction anthropometric indices
- Body mass index
- Fat and fat free mass indices
- Ponderal index
- Percentiles and Z-scores
- Anthropometry Video Resources
- Height procedure
- Protocol for measuring waist circumference
- Measuring hip circumference
- Weight and body composition procedure
Whole body DEXA scan
Dual-energy X-ray absorptiometry (DEXA) is an imaging technique. It provides whole body and regional estimates of the three main body components: fat, lean soft tissues and bone mineral mass. Some software can estimate visceral fat from the android/abdominal region (validated only in adults).
The instruments use a source that generates X-rays at two different energies, a detector, and an interface with a computer system for imaging the scanned areas of interest. The differential attenuation of the X-ray beam at these two energies is used to calculate the bone mineral content (BMC) and soft tissue composition in the scanned region. DEXA uses ionising radiation but the effective dose equivalents of contemporary instrumentation are below or equivalent to background levels, allowing for safe longitudinal studies in both children and adults.
There are two approaches:
- Some instruments (Hologic) have a switching pulse system that rapidly alternate the voltage of the X-ray generator, producing two beams of high and low energies. The attenuated X-rays that have passed through the participant are measured sequentially with a detector situated on the scanning arm above the participant.
- Other systems (GE Lunar and Norland), use X-rays which are produced by a constant-potential X-ray generator, and the beam is separated into high and low energy regions by k-edge filtration. The attenuated X-rays that have passed through the body are measured with an energy discriminating detector.
The difference in attenuation between the two energy peaks is particular to each element, and thus to each tissue. In all systems, the differential attenuation of the two energies is used to estimate bone mineral content and soft tissue composition.
There are different DEXA technologies:
- “pencil beam” DEXA, the first and original DEXA method (old technology), uses a singular beam of X-ray to produce an image, has a slower scanning time, but considered highly precise for bone assessment.
- “fan beam” (wide angle and narrow angle) DEXA system's have much faster scanning times, but may suffer from issues of magnification/distortion.
Calibration procedures
DEXA manufacturers have different quality assurance (QA) and quality control (QC) procedures. These include the system’s calibration as well as testing some software features.
- Instrument calibration is carried out by either an external calibration scan with a phantom calibration standard which tests the mechanical operation of the DEXA machine; or an internal calibration that checks each pixel measurements using a rotating internal wheel/drum.
- A separate phantom is used to also test the system performance over time by detecting changes in bone mineral density (BMD) values as well as monitoring short term and long term precision in vitro.
- Phantoms with known BMC, BMD and area mimic a region of the human skeleton (e.g. spine). They often resemble the human skeleton embedded in epoxy resin or submerged in water to simulate soft tissue. The phantom can be formulated to have a specific body composition.
- QC phantoms test both machine parameters and software features of edge detection and analysis. The purpose of this type of QA scanning is to detect any machine calibration failures or drifts occurring over a period of time, as well as changes resulting from maintenance and repair of the DEXA machine.
- The phantom should be rescanned multiple times (10 times) after the instrument installation to define the mean values of the measured BMD, BMC and area.
- The phantom should also be rescanned 10 times after service and any inspections from the radiation protection services/advisor.
Measurement procedures
Training in DEXA operation, positioning of the participants and data management is essential to obtain reliable data. Training is generally provided by each company along with an electronic standard operating manual embedded in the DEXA software.
The measurement procedure is similar for each instrument:
- Before the scan, participants should wear loose, comfortable clothing (tight elasticated trousers can affect the assessment of subcutaneous fat in the android region if using latest software) or changed into hospital gowns. Participants should avoid wearing clothing containing metal materials (e.g. underwired bras, zips etc.) as this material is thick and it will be interpreted as bone.
- Other checks include: pregnancy status, whether they have had medical/X-rays procedures including computer tomography (CT), and received any contrast media (e.g. barium, gadolinium etc.) as the scan would need to be postponed.
- During the scan, the participant lies on the scanning bed and is scanned in a straight line from head to toe.
- The X-ray source is positioned beneath the scanning bed.
- The scan normally takes 5-20 minutes, depending on the instruments and instruments' settings used (e.g. scan mode and the thickness of the tissue of the individual).
- Participant is to be positioned in the centre of the table, aligned with the long axis of the scanner, with their head near the head end of the table.
- The head should face straight up, not turned to the left or right.
- If required for comfort, especially if scanning older and frail individuals, radiolucent pillows can be used. If other types of pillows are used, the software might interpret this material as soft tissue (see Figure 1). Newer software has now features that enable the removal of these types of artefacts. Other artefacts, e.g. hip replacements are automatically removed by the software.
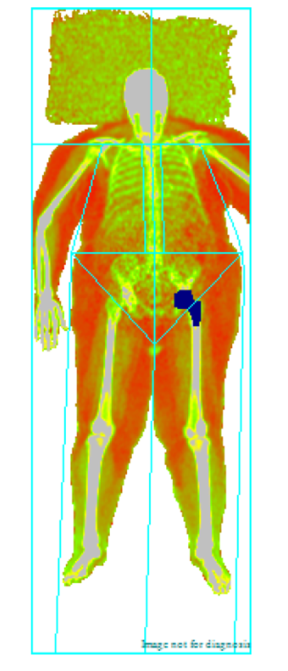
Figure 1 Showing artefacts: pillow and hip replacement.
Source: MRC Epidemiology Unit.
- The legs and feet should be positioned together with a fabric strap around the ankles to help prevent movement.
- Feet should be kept relaxed with the toes pointed upwards.
- Hands should be positioned with palms flat against the scanning bed. Space should be maintained between the arms and the trunk when possible. If this is not possible the hands may be placed in a lateral position next to the hips (palm to thigh position, see Figure 2). Hands should not be tucked under the hips.
- If the participant is still too broad to fit within the scanning area, apply the symmetry method per Figure 2 by firstly removing the left arm from the scanning area. For much larger individuals, the half body symmetry method might be necessary. Use the right side of the body when the participant is too broad for the table and carry out a half body scan.
- For participants who are too tall to fit within the scanning limits, they can be instructed to flex their feet when the scanning arm (detector) reaches their knees.
- To avoid movement artefacts, participants should not be engaged in conversation.
- When performing a follow up scan, the participant is to be repositioned in the same manner as per baseline where possible to obtain accurate data.
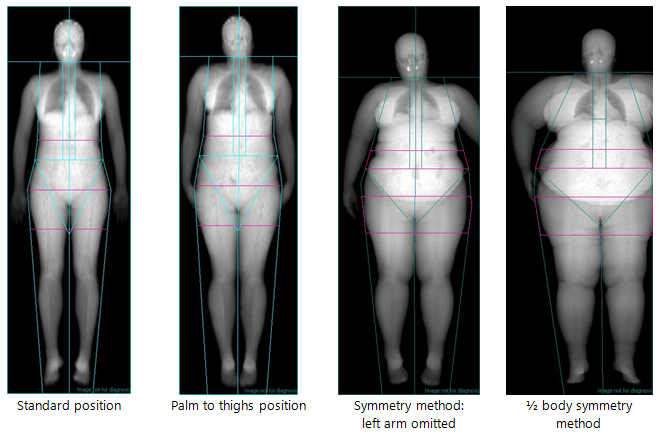
Figure 2 Body positions for DEXA scan.
Source: MRC Epidemiology Unit.
DEXA estimates bone mineral mass, lean mass and fat mass from the differential absorption of X-rays of two different energies using the instrument's specific algorithms. Manufacturers of DEXA systems also include correction algorithms for the effect of body thickness.
Assumptions associated with DEXA include: the assumed constant attenuation (R) of fat (R = 1.21) and of bone mineral content; minimal effects of hydration on lean tissue estimates.
Setting regions of interest (ROIs)
Different DEXA systems have an automated placement/demarcation of the boundaries of the body regions. Although, readjustments may be required and the standardised protocol in Figure 3 can be adopted.
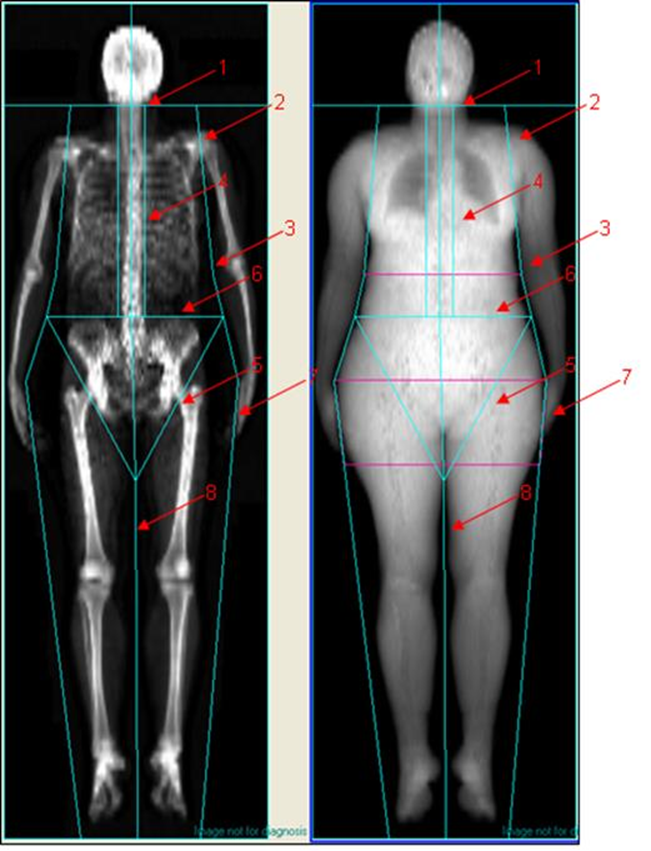
1: Head: the Head cut is located immediately below the chin.
2: Left and right arm: Both arm cuts pass through the arm sockets and are as close to the body as possible.
3: Left and right forearm: Both forearm cuts are as close to the body as possible and separate the elbows and forearms from the body.
4: Left and right spine: Both spine cuts are as close to the spine as possible without including the rib cage.
5: Left and right pelvis: both pelvis cuts pass through the femoral necks and do not touch the pelvis.
6: Pelvis top: The pelvis top is immediately above the top of the pelvis.
7: Left and right leg: Both leg cuts separate the hands and forearms from the legs.
8: Centre leg: The Centre leg cut separates the right and left leg.
Figure 3 Standard protocol for regions of interest (ROIs).
Source: MRC Epidemiology Unit.
Raw data
DEXA data are stored in databases inbuilt within the DEXA systems such as Microsoft Access and SQL. A data extraction tool can be set up to access the raw data and reconstruct body composition variables where necessary.
The raw data includes estimates of:
- Total body fat mass (g)
- Total bone mineral content (g)
- Total body lean mass (g)
- Body composition of tissues in specifically defined regions as per Figure 4
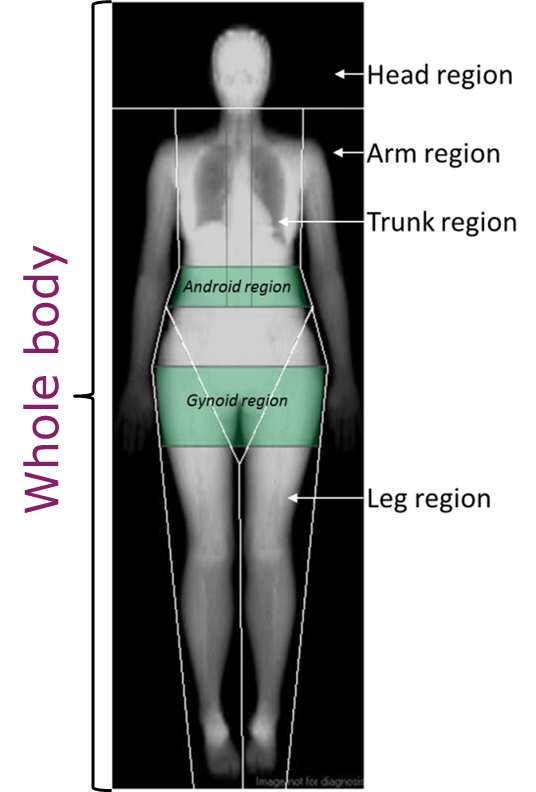
Figure 4 Locations of body composition estimations (e.g. whole, android region etc.).
Source: MRC Epidemiology Unit.
Bone mineral density standard scores
DEXA also estimates bone mineral density T-score and Z-score.
T-score
- A T-score shows how much the BMD of an individual varies from the BMD of an average young adult of the same sex, who has reached peak bone mass.
- Table 1 shows cut off points for BMD T-scores indicating osteoporosis or low BMD.
- Hip and spine scans are generally used for diagnosis of osteoporosis and low BMD
Table 1 World Health Organization cut off values to indicate presence of osteoporosis.
| T-score | Interpretation according to WHO criteria |
|---|---|
| Above -1 | Bone density is considered normal |
| Between -1 and -2.5 | Sign of osteopenia, a condition in which bone density is below normal an may lead to osteoporosis |
| Below -2.5 | Indicates presence of osteoporosis |
Adapted from: [4].
Z-score
- A Z-score is helpful for looking at the bone density of children and young adults, who have not reached peak adult bone mass.
- The Z-score is the number of units above or below what is normally expected for someone of the same age, sex, weight and ethnic origin. The results also need to be interpreted in relation to height.
- A Z-score of more than 2 standard deviations below other individuals of the same age should be followed up and referred to a medic/general practitioner.
Body composition variables when symmetry method is applied
Some software allows automated estimations of body composition for scans where the symmetry method was applied (e.g. arm omitted from scanning area or half-scan analysis). However, it is preferable to switch this feature off as the estimation can occur even if, for example, small tissue is clipped from the scanning area.
The following steps can be followed to rebuild an individual’s body composition data, depending on which regions are omitted from the scan. After the missing tissue has been rebuilt, percentage body fat can be derived.
a) Calculations for symmetry method when the left arm omitted is from scanning area
The procedure below removes the bone, the fat and the lean masses of the left arm from total mass, left total mass and left arm mass values and replaces it with the right arm values.
- Total bone mass = (Total bone mass – left arm bone mass) + Right arm bone mass
- Total fat mass = (Total fat mass – left arm fat mass) + Right arm fat mass
- Total lean mass = (Total lean mass – left arm lean mass) + Right arm lean mass
- Left total bone mass = (Left total bone mass – left arm bone mass) + Right arm bone mass
- Left total fat mass = (Left total fat mass – left arm fat mass) + Right arm fat mass
- Left total lean mass = (Left total lean mass – left arm lean mass) + Right arm lean mass
- Left arm bone mass = Right arm bone mass
- Left arm fat mass = Right arm fat mass
- Left arm lean mass = Right arm lean mass
b) Calculations for 1/2 body symmetry method
- Total bone mass = (Total bone mass – left total bone mass) + Right total bone mass
- Total fat mass = (Total fat mass – left total fat mass) + Right total fat mass
- Total lean mass = (Total lean mass – left total lean mass) + Right total lean mass
- Left total bone mass = Right total bone mass
- Left total fat mass = Right total fat mass
- Left total lean mass = Right total lean mass
- Left arm bone mass = Right arm bone mass
- Left arm fat mass = Right arm fat mass
- Left arm lean mass = Right arm lean mass
- Left leg bone mass = Right leg bone mass
- Left leg fat mass = Right leg fat mass
- Left leg lean mass = Right leg lean mass
c) Calculation of body composition following rebuild
Percentage body fat can then be derived using the following calculations:
- Firstly regenerate the total mass using the estimates above
- Total mass in kg = ((Total Bone Mass + Total Fat Mass + Total Lean Mass)/1000)
- Percentage body fat = (100*Total Fat Mass)/(Total Mass in kg*1000)
Visceral fat estimates
Different manufacturer have developed algorithms to estimate visceral fat from the android/abdominal region by estimating the subcutaneous fat on each side of the abdominal wall thickness (Figure 5). This measurement is used to extrapolate the amount of subcutaneous fat in the abdominal/android region using appropriate modelling (e.g. circular or spherical models). Visceral fat is derived by subtracting the estimated abdominal subcutaneous fat from the total android/abdominal fat mass.
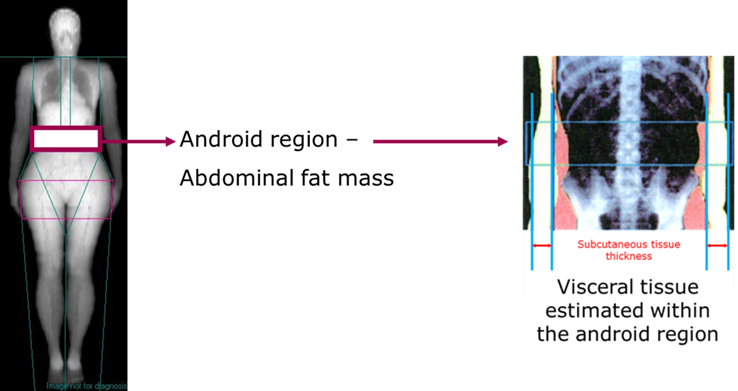
Figure 5 Visceral fat estimation within the android/abdominal region.
Source: MRC Epidemiology Unit.
Derived variables
Further data can be derived, which are not given by the software automatically:
- Appendicular lean mass (g) = (lean mass in the limbs (arms and legs) in g - lean mass in the trunk and head in g). This can be used as a proxy measure for skeletal muscle and it has been used to study sarcopenia
- Peripheral fat mass (g) = (fat mass in the limbs in g - fat mass in the trunk and head in g)
- Abdominal subcutaneous fat (g) = (Android fat mass in g - visceral fat mass in g)
- Lower body fat (g) = [Total fat mass g - (Trunk fat mass g + arms fat mass g)]
Harmonisation of data from different DEXA manufacturers
There are published translation regression equations to tackle the systematic differences in the absolute values of body composition variables between different manufactures [2, 9]. However, these equations have been derived from healthy individuals and they might not be generalisable to other populations. Cross-calibration study of different instruments is therefore recommended to derive translation regression equations.
When replacing an instrument, the ISCD (International Society of Clinical Densitometry) guidelines recommend carrying out cross-calibrations between the old and new instruments in at least 30 participants scanned on each instrument, twice on the new instrument to test precision and accuracy and derived cross-calibration equations.
DEXA was created for and continues to be used as a clinical tool to assess bone mineral density and bone mineral content to diagnose osteoporosis (thinner bones). Other body sites (e.g. spine, forearm and hip scans) are used for this purpose.
It is typically used in research settings to assess body composition in:
- Large-scale observational cohort studies.
- Studies undertaking association analyses between exposure(s) and outcome(s).
- Interventions and randomised controlled trials to examine intervention or treatment efficacy.
- Validation studies as a reference method to evaluate simpler body composition measurements (e.g. skinfolds; BIA) when the criterion method is not applicable or available.
- Bone mineral content by DEXA is also used to derive the 4-component model, the criterion method for assessment of body composition, together with other body composition methods.
An overview of the characteristics of whole body DEXA scanning is outlined in Table 3.
Strengths
- DEXA has the advantage of requiring little cooperation, being relative quick, 5-20 minutes, and having a low radiation dose. It is also possible to carry out DEXA measures in a mobile van.
- It is highly precise (see Table 2 for examples of GE Lunar Prodigy and GE iDEXA).
- Able to estimate overall body fat as well as body fat patterning and distribution as shown in Figure 6.
Table 2 Precision of two DEXA instruments.
| Total body fat CV% | Regional body fat CV% | Pixel (mm) | |
|---|---|---|---|
| Prodigy | 1.9 | 1.2 – 4.4 | 4.8 / 13.0 |
| iDEXA | 0.9 | 0.9 – 2.4 | 2.4 / 3.04 |
CV: Coefficient of variation.
Adapted from: [3].
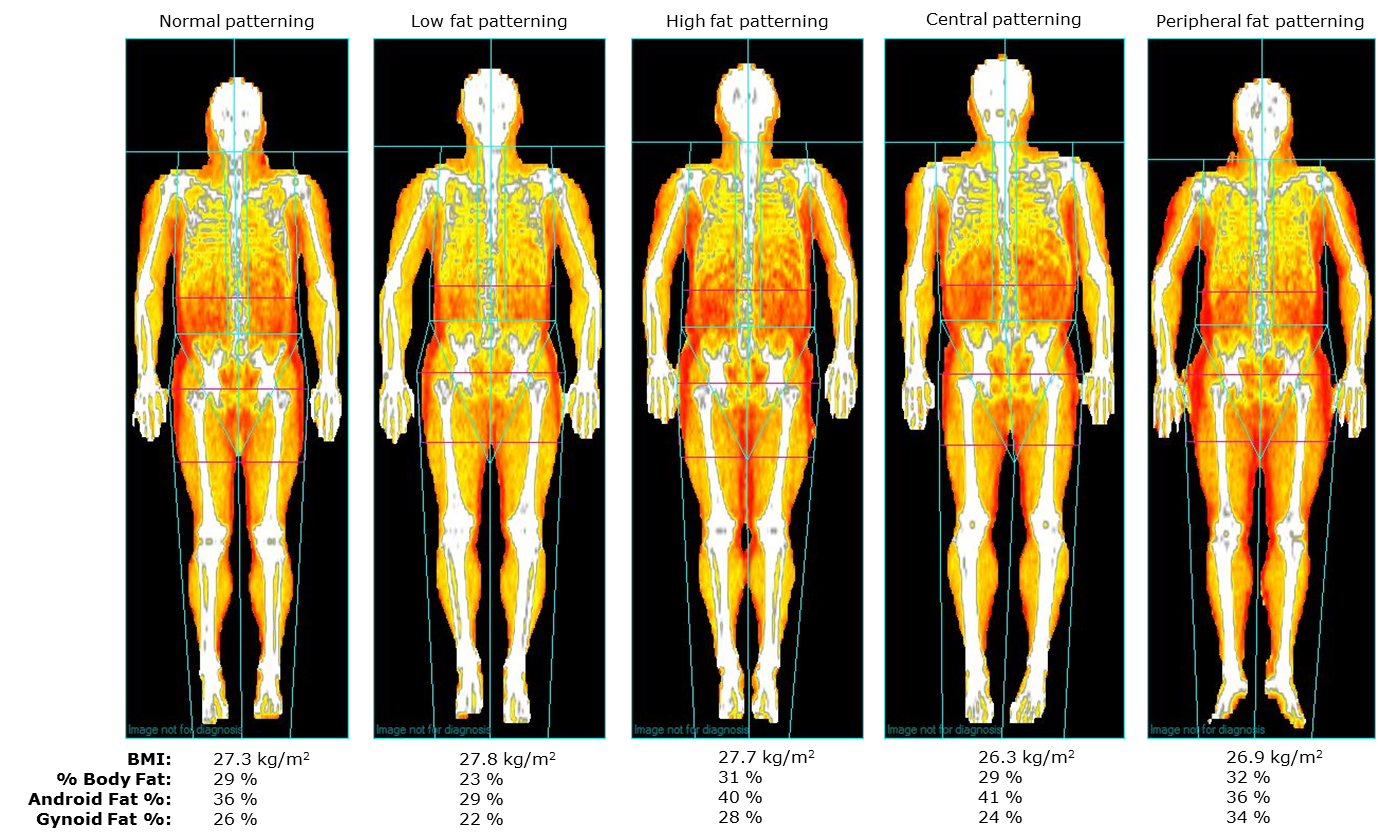
Figure 6 Fat patterning and distribution using DEXA.
Source: MRC Epidemiology Unit.
Limitations
- DEXA estimates of fat mass are influenced by ‘trunk thickness’ with the error increasing as the individual’s trunk thickness increases. In longitudinal studies of persons who undergo significant changes in body composition, DEXA measures can be biased and display systematic differences.
- Marked differences in the hydration of lean tissue may affect the accuracy of body composition measures, especially in infants as they have a higher degree of lean tissue hydration than adults.
- Marked systematic differences in bone and soft tissue values are found between three commercial systems (Hologic, GE and Norland) due to differences in calibration, bone edge detection, and correction factors [5].
- Software updates can cause significant changes to soft tissue values and BMD.
- Bias varies by different beam technology (pencil beam – old technology vs fan beam systems), instruments, software, age, fatness and underlying disease state.
Table 3 Characteristics of whole body DEXA scanning.
| Consideration | Comment |
|---|---|
| Number of participants | Large |
| Relative cost | Medium |
| Participant burden | Low |
| Researcher burden of data collection | Low |
| Researcher burden of coding and data analysis | Medium |
| Risk of reactivity bias | No |
| Risk of recall bias | No |
| Risk of social desirability bias | No |
| Risk of observer bias | No |
| Space required | Medium |
| Availability | High |
| Suitability for field use | Possible only using mobile van |
| Participant literacy required | No |
| Cognitively demanding | No |
Considerations relating to the use of DEXA for anthropometry in specific populations are described in Table 4.
Table 4 Anthropometry by whole body DEXA scan in different populations.
| Population | Comment |
|---|---|
| Pregnancy | Not suitable due to the unknown adverse effects of the radiation dose to the fetus. |
| Infancy and lactation | Swaddling techniques are recommended in infants and the measurements can be carried out while the infant is asleep. However, the accuracy of regional soft tissue measurements can be affected if swaddling is used as the arm regions will be incorporated with the thigh regions. |
| Toddlers and young children | This technique may be impractical in young children as the protocol requires the participant to stay as still as possible as movements may invalidate the results. Feasible to use down to 4 years and in small infants. |
| Adolescents | Suitable. |
| Adults | Suitable. |
| Older Adults | Suitable. |
| Ethnic groups | Reference data for body composition not available for some ethnic groups. |
| Other (obesity) | Most systems cannot accommodate individuals with BMI ≥35. Newer models can measure up to 200 kg. A half body scan is generally required in those individuals (see measurement procedure). This method provides valid estimates of body composition when compared to the criterion method. |
Safety and ethical considerations:
- Most countries require that the legal person responsible for the DEXA facility unit apply to the radiation protection regulatory body for authorization - either via registration or a licence.
- The relevant regulatory body will require information necessary to demonstrate the protection and safety of the practice. Typically, this includes information on the medical practitioners and technologists/operators involved; their education and training in radiation protection; details on the DEXA equipment and the room where it is to be located; and the facility’s radiation protection programme for staff, patients/study participants and general public protection.
- In both clinical and research environment, all medical exposures are required to be appropriately justified. The diagnostic benefit from DEXA must outweigh the radiation detriment that might ensue. In medical research, the benefit from the use of radiation is expected to be accrued by society, such as through improved health care options. The use of DEXA procedures in this role must normally also be justified by an ethics committee.
- In the UK, the IR99 (statutory regulations for the use and control of ionising radiation) and IRMER (Ionising Radiation Medical Exposure Regulations) 2000/2006 regulations (legislation intended to protect the patient/participant from the hazard associated with ionising radiation) are applied.
Other procedural considerations:
- Always compare the sum of DEXA parts (total DEXA weight) and scale weight to assess quality control of DEXA measurements
- Always cite software version and hardware version when publishing DEXA data
- If using DEXA in multicomponent models use the following equations:
- Lohman and Going [7]
- Wang et al. [10]
- Withers et al. [12]
- For QC purposes, it is recommended that the demarcations of the regional boundaries (ROIs) are checked by a trained technician/operator, who did not carry out the scan.
Refer to section: practical considerations for objective anthropometry
- DEXA system
- Trained operators
- Velcro straps
- DEXA record book to record each exposure
- Tissue paper
- Non-alcoholic wipes
- Radiation Protection policy that covers operators and patients/participants
- Access to a Radiation Protection Advisor
- In some countries, this type of measurements can only be made by a licensed X-ray technician
- Data manager
- Radiation badges to monitor the cumulative dose in the DEXA suite; these are normally provided by the Radiation Protection Advisor
A method specific instrument library is being developed for this section. In the meantime, please refer to the overall instrument library page by clicking here to open in a new page.
- Heymsfield SB, Lohman TG, Wang Z, Going SB. Human Body Composition, Second Edition. Windsor ON. Human Kinetics. 2005
- Hull H, He Q, Thornton J, Javed F, Allen L, Wang J, et al. iDXA, Prodigy, and DPXL dual-energy X-ray absorptiometry whole-body scans: a cross-calibration study. Journal of clinical densitometry : the official journal of the International Society for Clinical Densitometry. 2009;12(1):95-102. Epub 2008/11/26.
- Kaminsky LA, Ozemek C, Williams KL, Byun W. Precision of total and regional body fat estimates from dual-energy X-ray absorptiometer measurements. The journal of nutrition, health & aging. 2014;18(6):591-4. Epub 2014/06/21.
- Kanis JA et al. The diagnosis of osteoporosis. Journal of Bone and Mineral Research, 1994, 9: 1137–1141.
- Laskey MA. Dual-energy X-ray absorptiometry and body composition. Nutrition. 1996;12(1):45-51. Epub 1996/01/01.
- Lee SY, Gallagher D. Assessment methods in human body composition. Current opinion in clinical nutrition and metabolic care. 2008;11(5):566-72. Epub 2008/08/08.
- Lohman TG, Going SB. Multicomponent models in body composition research: opportunities and pitfalls. Basic Life Sci. 1993;60:53-8.
- Rothney MP, Brychta RJ, Schaefer EV, Chen KY, Skarulis MC. Body composition measured by dual-energy X-ray absorptiometry half-body scans in obese adults. Obesity. 2009;17(6):1281-6. Epub 2009/07/09.
- Soriano JM, Ioannidou E, Wang J, Thornton JC, Horlick MN, Gallagher D, et al. Pencil-beam vs fan-beam dual-energy X-ray absorptiometry comparisons across four systems: body composition and bone mineral. Journal of clinical densitometry : the official journal of the International Society for Clinical Densitometry. 2004;7(3):281-9. Epub 2004/08/21.
- Wang Z, Pi-Sunyer FX, Kotler DP, Wielopolski L, Withers RT, Pierson RN, Heymsfield SB. Multicomponent methods: evaluation of new and traditional soft tissue mineral models by in vivo neutron activation analysis. Am J Clin Nutr. 2002; 76(5): 968-974.
- Wells JC, Fewtrell MS. Measuring body composition. Archives of disease in childhood. 2006;91(7):612-7. Epub 2006/06/23.
- Withers RT, Smith DA, Chatterton BE, Schultz CG, Gaffney RD. A comparison of four methods of estimating the body composition of male endurance athletes. Eur J Clin Nutr. 1992; 46(11): 773-784.
- Williams JE, Wells JC, Wilson CM, Haroun D, Lucas A, Fewtrell MS. Evaluation of Lunar Prodigy dual-energy X-ray absorptiometry for assessing body composition in healthy persons and patients by comparison with the criterion 4-component model. Am J Clin Nutr. 2006;83(5):1047-54. Epub 2006/05/11.
- http://www.iscd.org/
- http://www-pub.iaea.org/MTCD/publications/PDF/Pub1479_web.pdf
- http://nt-cmb.medun.acad.bg:8080/jspui/bitstream/10861/265/3/Mihail-Boyanov_Quolity_assurance_20-06-2013.pdf
