- Introduction to Subjective Methods
- Birth weight
- Body shape
- Weight and height
- Waist and hip circumference
- Introduction to Objective Methods
- Simple measures - stature
- Simple measures - weight
- Simple measures - circumference
- Simple measures - arm anthropometry
- Simple measures - skinfolds
- Simple measures - abdominal sagittal diameter
- Simple measures - head circumference
- Bioelectric impedance analysis
- Multi-component models
- Hydrostatic underwater weighing
- Air displacement plethysmography
- Hydrometry
- Whole body DEXA scan
- Near infrared interactance
- Whole body counting of total body potassium
- 3d photonic scan
- Magnetic resonance imaging (MRI) / Magnetic resonance spectroscopy (MRS)
- Total body electrical conductivity (TOBEC)
- Computed tomography (CT)
- Ultrasonography
- Introduction anthropometric indices
- Body mass index
- Fat and fat free mass indices
- Ponderal index
- Percentiles and Z-scores
- Anthropometry Video Resources
- Height procedure
- Protocol for measuring waist circumference
- Measuring hip circumference
- Weight and body composition procedure
Simple measures - head circumference
Head circumference (HC) is a measurement of the head around its largest area, typically measured on infants and children until the age of five years as part of routine child care. It measures the distance from above the eyebrows and ears and around the back of the head.
In children, this measurement forms part of a growth assessment to provide information on health, development and nutritional status (other measurements include height and weight). HC and the ratio between HC and weight for example, may also detect any abnormal brain or skull growth (e.g. hydrocephalus, microcephaly, macrocephaly).
HC is a simple, inexpensive and easily accessible tool for monitoring brain development and identifying infants at risk of neurodevelopmental disorders (Garcia-Alix et al., 2004). HC is often used in infants born small for gestational age (SGA). SGA babies and infants with a birth weight less than the 10th percentile are at an increased risk of perinatal morbidity, continued short stature, and metabolic alterations later on in life (Cho and Suh, 2016). Studies have shown that SGA infants present with a higher rate of growth for head circumference compared to their appropriate for gestational age (AGA) peers – i.e. SGA infants try to catch-up with AGA infants to undo the effects of nutritional insult experienced during gestation (Kaur et al., 2011).
HC is typically measured using a flexible but non-stretch tape, such as the Seca 212 measuring tape or Lasso-o Child Growth Foundation tape. The tape measure should be checked for correct assembly and any damage before each use.
Protocol
- The child should be standing, seated or seated on parent/guardian's lap depending on age and ability.
- Any hair ornaments or braiding should be removed if possible.
The tape should then be placed over the child’s head above the ears and eyebrows on the most anterior protuberance of the forehead (frontal bone) and around the occipital prominence at the back of the head.
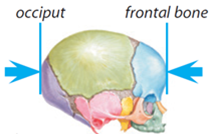
Figure 1 The occipital and frontal bones of the human skull.
Source: Infant and Toddler Forum
- Aim to measure the largest circumference possible
- The tape should be pulled tight so that any hair is compressed
- The measurement should be read and recorded to the nearest millimetre
- Repeat the measurement and if there is a difference of >0.5cm, a third should be taken
- The tapes typically show both centimetres and inches, ensure that the measurement is taken using the metric scale
- If the infant/child has an abnormally shaped head (eg. craniosynostosis or a low airline (Saethe-Chotzen syndrome), ensure that the tape is placed over the largest measurable circumference
- HC should not be carried out before 36 hours of age due to scalp oedema, preferably to be assessed at 7-10 days of age

Figure 2 Recording head circumference.
Source: MRC Epidemiology Unit.
HC is used in clinical practice, in nutritional surveys and in epidemiological studies in combination with other anthropometric measures such as height and weight to provide an assessment of growth and development.
The relationship between HC and weight for example can identify if there is a need for further monitoring or investigation; a small head circumference with a low weight needs a different approach compared to a small head with a normal weight (GOSH Clinical Guidelines Online, 2017). Some studies have shown that HC standard deviation scores (or Z-scores) are highly correlated with those for height and weight, and this suggests that body size should be taken into account when interpreting the HC of a child (Geraedts et al., 2011).
Plotting HC on child growth standard charts can give an immediate indication of whether the child’s head, and therefore brain, is growing and a rate which is expected.
Growth Charts
Standardized growth charts are used to plot HC each time it is measured throughout the first years of life. This can show how HC is changing over time and can highlight if HC is increasing too quickly or not quick enough.
The World Health Organization provides access to such charts up to the age of 5 years:
- Head circumference-for-age Girls (birth to 5 years)
- Head circumference-for-age Boys (birth to 5 years)
However, these charts must be interpreted together with age and special consideration must be taken for infants who were born prematurely. For example, an infant born 6 weeks early (at 34 weeks gestation) will have a corrected age of 6 weeks less than his/her actual age since birth. Their measurements should be plotted on the chart at their actual age, with a horizontal line drawn back to their corrected age. Adjustments for prematurity to be made until they reach one year of age. Early year UK WHO growth charts (rcpch.ac.uk)
The head circumference-for-age is typically used together with other growth indices to assess infants’ growth and development. It is often used in clinical settings as part of health screening for potential developmental or neurological disabilities in infants and young children.
This index is expressed in percentiles (percentage of median) and can be assessed by the percentile point achieved by a child relative to the healthy children of that age and gender in the same population. Median is regarded as a reference value, and 3rd and 97th percentiles as thresholds to indicate abnormally low or abnormally high values.
It can also be expressed as a Z-score derived by using the formula:
(Measured value – Average value in the reference population) / Standard deviation of the reference population
The WHO growth standard for head circumference for age is used for its interpretation.
Typically, an infant with a HC >97th percentile is considered to present with macrocephaly, while a HC of <3rd percentile is considered as microcephaly (Daymont et al., 2012).
An overview of head circumference methods is outlined in Table 1.
Strengths
- Quick to measure
- Non-invasive
- Easily accessible, inexpensive equipment
Limitations
- Sometimes difficult to measure on non-cooperative infants
- Requires access to growth charts and/or other measures for interpretation of results
- Inaccurate to measure before 36 hours of age due to scalp oedema
Table 1 Characteristics of head circumference methods.
| Characteristic | Comment |
|---|---|
| Number of participants | High |
| Cost of development | Low |
| Cost of use | Low |
| Participant burden | Low |
| Researcher burden of data collection | Low |
| Researcher burden of coding and data analysis | Low |
| Risk of reactivity bias | No |
| Risk of recall bias | No |
| Risk of social desirability bias | No |
| Risk of observer bias | Yes |
| Participant literacy required | No |
| Cognitively demanding | No |
| Suitable for use in the field | Yes |
Considerations relating to the use of head circumference methods in specific populations are described in Table 2.
Table 2 Use of head circumference methods in different populations.
| Population | Comment |
|---|---|
| Pregnancy | Typically used in infancy and childhood, but it is suitable to use in this population. |
| Infancy and lactation | Suitable. |
| Toddlers and young children | Suitable. |
| Adolescents | Typically used in infancy and childhood, but it is suitable to use in this population. |
| Adults | Typically used in infancy and childhood, but it is suitable to use in this population. |
| Older Adults | Typically used in infancy and childhood, but it is suitable to use in this population. |
| Ethnic groups | Suitable as WHO HC for age can be used in infants and children of different ethnic backgrounds. |
| Other (obesity) | Typically used in infancy and childhood, but it is suitable to use in this population. However, it can be used in overweight and obese children and infants. |
Refer to section: practical considerations for objective anthropometry
- Head circumference tape (in cms)
- WHO Growth Charts
- Data entry form (either paper or computerised)
- Trained research staff
- Standard operating procedures for data collection
- Standard operating procedures for data entry and data cleaning
A method specific instrument library is being developed for this section. In the meantime, please refer to the overall instrument library page by clicking here to open in a new page.
- Cho WK, Suh BK. Catch-up growth and catch-up fat in children born small for gestational age. Korean J Pediatr. 2016 Jan;59(1):1-7. PubMed PMID: 26893597. Pubmed Central PMCID: 4753194. Epub 2016/02/20. eng.
- Clayton PE, Cianfarani S, Czernichow P, Johannsson G, Rapaport R, Rogol A. Management of the child born small for gestational age through to adulthood: a consensus statement of the International Societies of Pediatric Endocrinology and the Growth Hormone Research Society. J Clin Endocrinol Metab. 2007 Mar;92(3):804-10. PubMed PMID: 17200164. Epub 2007/01/04. eng.
- Cragan JD. National Center on Birth Defects and Developmental Disabilities, Surveillance for Microcephaly 2016 [07/11/2017]. Available from: https://www.cdc.gov/ncbddd/birthdefects/documents/surveillance-microcephaly-webinar.pdf.
- Daymont C, Zabel M, Feudtner C, Rubin DM. The test characteristics of head circumference measurements for pathology associated with head enlargement: a retrospective cohort study. BMC Pediatr. 2012 Jan 23;12:9. PubMed PMID: 22269214. Pubmed Central PMCID: 3331824. Epub 2012/01/25. eng.
- Forum IaT. Growth and its measurements, Toddler Factsheet 3.1 2009 [07/11/2017]. Available from: https://www.infantandtoddlerforum.org/media/upload/pdf-downloads/3.1_Growth_and_its_Measurement.pdf.
- Garcia-Alix A, Saenz-de Pipaon M, Martinez M, Salas-Hernandez S, Quero J. [Ability of neonatal head circumference to predict long-term neurodevelopmental outcome]. Rev Neurol. 2004 Sep 16-30;39(6):548-54. PubMed PMID: 15467994. Epub 2004/10/07. Utilidad del perimetro cefalico en el recien nacido para anticipar problemas en el neurodesarrollo. spa.
- Geraedts EJ, van Dommelen P, Caliebe J, Visser R, Ranke MB, van Buuren S, et al. Association between head circumference and body size. Horm Res Paediatr. 2011;75(3):213-9. PubMed PMID: 21311161. Epub 2011/02/12. eng.
- gosh.nhs.uk
- Kaur H, Bhalla AK, Kumar P. Longitudinal growth of head circumference in term symmetric and asymmetric small for gestational age infants. Early Hum Dev. 2012 Jul;88(7):473-8. PubMed PMID: 22178000. Epub 2011/12/20. eng.
- May L. Head circumference: measuring a child Great Ormond Street Hospital, NHS Foundation Trust Website2004 [07/11/2017]. Available from: http://www.gosh.nhs.uk/health-professionals/clinical-guidelines/head-circumference-measuring-child.
- National Institute for Health Research SBRC. Proceedure for Measuring Circumferences in Children 2015. Available from: http://www.uhs.nhs.uk/Media/Southampton-Clinical-Research/Procedures/BRCProcedures/Procedure-for-circumference-measurements-of-children.pdf.
- NHANES. National Health and Nutrition Examination Survey (NHANES); Anthropometry Proceedures Manual 2009 [07/11/2017]. Available from: https://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/bodymeasures_09.pdf.
- Ochiai M, Nakayama H, Sato K, Iida K, Hikino S, Ohga S, et al. Head circumference and long-term outcome in small-for-gestational age infants. J Perinat Med. 2008;36(4):341-7. PubMed PMID: 18598125. Epub 2008/07/05. eng.
- Plus M. Head Circumference 217 [07/11/2017]. Available from: https://medlineplus.gov/ency/article/002379.htm.
